Better outcomes for patients with wrist fracturent-centred research
Steve Watts is active. He plays squash and is converting a bedroom into an office. He has to wear compression gloves to do the normal work of hammering and painting because of the pain and lack of mobility that comes with osteoarthritis. His only other option is bone fusion.
Thirty years ago, Steve fractured his wrist after a fall from a horse on his father’s farm. The impact of that fall continues today. “Having just begun the process of having osteoarthritis, I know how important my hands are and having that movement,” says Steve. “Having that pain there - in the background - is the biggest negative impact to one’s life.”
Breaking a wrist is one of the most common causes of emergency visits in Canada. Wrist fractures account for 14 percent of injuries to seniors and 22 percent for adolescents. After an emergency visit for a wrist fracture, a complete recovery is complicated and in many cases patients live with chronic pain, malunion and abnormal kinematics for the rest of their lives.
A collaborative, crossfaculty team led by Principal Investigator, Emily Lalone, PhD, Assistant Professor in Department of Mechanical & Materials Engineering, received funding from Western University’s Bone and Joint Institute (BJI) Catalyst Grant Program to study the issue. Lalone and Dr. Joy MacDermid, professor and co-director of the Clinical Research Lab within the Roth McFarlane Hand & Upper Limb Centre, and their team are looking at diagnostic tools to characterize the effects of wrist fractures on joint mechanics early on to reduce the prevalence of post-traumatic osteoarthritis.
“Fracture complications lead to mal-tracking and malwear within the joint that cause serious conditions, like osteoarthritis,” says Lalone. “The rates of arthritis following orthopaedic injury of the wrist are unacceptably high — a substantial proportion of post-traumatic osteoarthritis is preventable”.
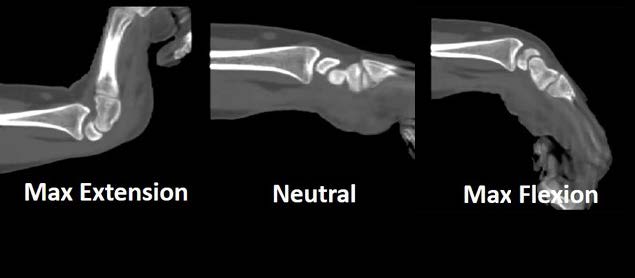
Following fracture, surgeons monitor the joint alignment using static x-ray. The difficulty however is that patients experience pain when they “load” or use their hands and wrist not necessarily when their hand is lying flat on the x-ray detector. “It is regular practice to examine a fracture using an x-ray,” says Lalone, “but 2D and even 3D imaging have limitations. Neither adequately show joint mechanics or harmful malunion.” In addition to these imaging limitations, most fractures are clinically treated with a cast, but with a static wrist, patients do not experience the symptoms that could indicate malunion or misalignment. Lalone and Dr. MacDermid aim to standardize the analysis of fractures and help determine optimal treatment by obtaining functional range of motion and weight-bearing scans.
4D CT (3D CT + time) scanning to examine people after a fracture has healed can track the movement of wrists and identify hot spots of increased wear – highlighting mal-tracking issues. When combined with surveys about pain and mobility, Lalone and team can better understand which treatments are most successful — a cast or reconstructive surgery. So far, the team has obtained images from 110 individuals — half with no fracture and half post-fracture. This is the beginning of what will be a comprehensive database of risk injuries. They are using this database to develop protocols for positioning and loading of the wrist during 3D and 4D scanning. The goal is to create best practice guidelines that give clinicians the ability to make informed therapeutic decisions for their patients. The goal is to reduce longterm complications such as pain, lack of mobility and quality of life.
“It’s bench to bedside work,” says Lalone. “BJI aims to bring people from across campus to collaborate, and with our lab located just above our clinic, crossdisciplinary collaboration between clinicians and engineers for this project has been no exception. It’s been pivotal to our success.”
“One of the things we are proposing to do next is to introduce artificial intelligence (AI),” says Lalone. ”AI can sometimes see things we can’t. So, if you plug in prospective data, it will help us create two-year benefit grids that can estimate the likelihood for a patient to experience difficulties later on.” The team’s work has already led to three peerreviewed publications (accepted – publication pending) and four more papers are in preparation. Ultimately, for patients, their work means decreasing pain, avoiding a chronic disease and improving quality of life. For the healthcare system, the research may result in cost-savings by reducing the resources needed to treat patients over their lifetime.
“This research offers hope for people who are having the same problems as I am,” says Steve. “It will give physicians the ability to make better decisions based on the data. Research can lead to changes and treatments for conditions that no one has ever thought of before. One day, it can improve someone’s quality of life.”

